|
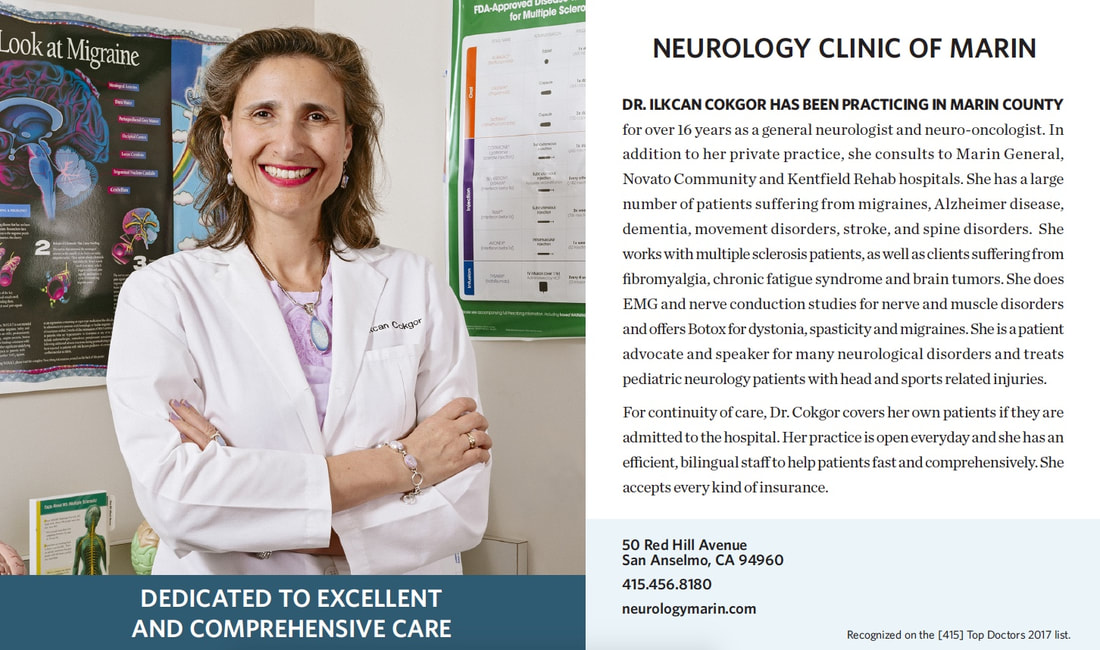
Dr. Ilkcan Cokgor, MD selected for inclusion in the
Nationwide Registries Top Doctors of America 2024 Honors Edition
For millions of individuals worldwide, migraines are not just occasional headaches but rather debilitating episodes that disrupt daily life. Migraines are a complex neurological disorder characterized by intense, throbbing headaches often accompanied by symptoms such as nausea, vomiting, light sensitivity, and visual disturbances. They can significantly impair a person's ability to carry out routine tasks, affecting their quality of life. Traditional treatments have often provided limited relief, prompting a search for more effective solutions. Prevention is key for individuals suffering from chronic migraines (experiencing headaches on 15 or more days per month for at least three months). One such breakthrough in migraine management comes in the form of CGRP (calcitonin gene-related peptide) receptor blocker medications in the treatment of both acute and chronic migraines. CGRP receptor blockers have emerged as a promising solution for this challenging patient population.
CGRP is a neuropeptide that plays a pivotal role in migraines. It is released during a migraine attack and is associated with the transmission of pain signals and inflammation in the brain. This discovery led to the development of CGRP receptor blocker medications. They are also known as CGRP antagonists or monoclonal antibodies, specifically designed to target the CGRP pathway. They block the receptors that CGRP binds to, inhibiting its effects on the brain. Traditionally, acute migraines have been treated with a combination of pain relievers, anti-nausea medications, and lifestyle modifications. While these approaches can be effective for some, they fall short for many others. CGRP receptor blockers offer a new avenue for acute migraine relief. These medications are administered through oral, sublingual, or nasal ways, providing rapid and targeted relief when used as a rescue medicine. They are administered through oral or subcutaneous injections when used as preventive drugs. Studies have shown that they can significantly reduce the severity and duration of migraine attacks, offering hope for those who have struggled with conventional treatments. Unlike traditional preventive medications that may have side effects or interactions with other drugs, CGRP receptor blockers are well-tolerated with very mild side effects. Possible side effects are constipation or dizziness. CGRP receptor blockers represent a significant advancement in the treatment of both acute and chronic migraines. By targeting the CGRP pathway, these medications offer new hope for individuals who have long grappled with the debilitating effects of this neurological disorder. As research in this field continues to evolve, we can anticipate even more refined and effective treatments, bringing us closer to a future where migraines no longer dominate the lives of those affected. If you or a loved one struggles with migraines, it may be worth discussing CGRP receptor blockers with your healthcare provider to see if they are a suitable option for you. Remember, relief might be closer than you think. A Ray of Hope: Leqembi and the New Wave of IV Medications in Alzheimer's Disease Treatment10/27/2023
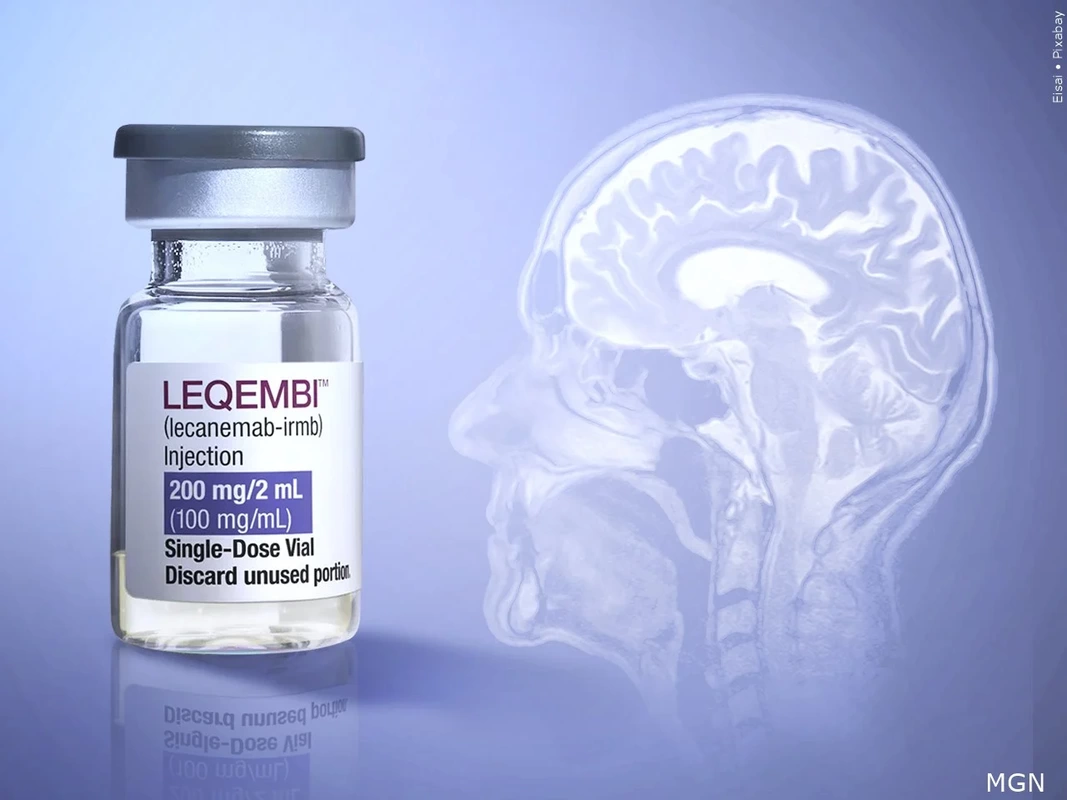
Alzheimer's Disease, a progressive neurodegenerative disorder, affects millions worldwide. Its hallmark features include cognitive decline, memory loss, and impaired daily functioning. Despite decades of research, a definitive cure or universally effective treatment has remained elusive. However, recent developments in intravenous medications offer a glimmer of hope for those affected by this devastating condition. Among the latest breakthroughs is Leqembi, an intravenous drug that holds promise in the battle against this neurological condition.
Leqembi (also known by its generic name, lecanemab) is a monoclonal antibody that targets beta-amyloid plaques—a critical pathological hallmark of Alzheimer's Disease. These plaques are abnormal accumulations of a protein fragment called beta-amyloid that accumulate in the brains of individuals with Alzheimer's. Administered intravenously, Leqembi specifically binds to beta-amyloid, effectively marking these plaques for removal by the body's immune system. This targeted approach holds immense promise in slowing down or potentially halting the progression of Alzheimer's. Leqembi's journey to approval involved rigorous clinical trials. Initial results have been encouraging, with some studies demonstrating a significant reduction in beta-amyloid plaque burden. Furthermore, early findings suggest potential cognitive benefits for some patients. While Leqembi represents a significant step forward in Alzheimer's research, it's important to note that it's not a cure-all. Alzheimer's is a complex disease with multiple underlying factors, and a comprehensive treatment approach may involve a combination of therapies. Leqembi is not alone in battling Alzheimer's through intravenous medications. Several other promising candidates are in various stages of development and clinical trials. These include aducanumab, donanemab, and gantenerumab, each targeting beta-amyloid in distinct ways. As with any medical treatment, Leqembi and similar intravenous medications may not suit everyone. Patients and caregivers should discuss openly with healthcare providers to understand the potential benefits, risks, and individualized treatment plans. The introduction of Leqembi and other intravenous medications marks an exciting chapter in the fight against Alzheimer's Disease. As research and clinical trials progress, the landscape of Alzheimer's treatment is evolving, bringing us closer to more effective therapies and, ultimately, a brighter future for individuals living with Alzheimer's Disease. In a world grappling with the challenges of obesity, it's essential to recognize that the impact of excess weight extends beyond physical health. Obesity has reached alarming proportions globally. The World Health Organization (WHO) states that over 650 million adults were obese in 2016. This epidemic poses risks to cardiovascular health and raises concerns about its impact on neurological well-being. Emerging research sheds light on the intricate relationship between being overweight and neurological disorders. The brain and body communicate through a complex network of signals. Adipose tissue, commonly called fat, secretes hormones and inflammatory substances. When in excess, these can disrupt this communication, leading to a cascade of effects on the brain.
Obesity is associated with chronic low-grade inflammation. This inflammation doesn't only affect joints or organs but can also extend to the brain. Studies suggest that it may contribute to the development and progression of neurological disorders, including Alzheimer's Disease, multiple sclerosis, and Parkinson's Disease. Obesity-induced inflammation may exacerbate these conditions, potentially accelerating their progression. Obesity often leads to insulin resistance, a condition where cells become less responsive to insulin. Hence, this contributes to diabetes but also affects cognitive function. Some studies suggest that insulin resistance may be a precursor to cognitive decline and conditions like Alzheimer's. Obesity also alters the balance of hormones in the body, including those responsible for mood regulation. This hormonal imbalance may increase the risk of mental health conditions, such as depression and anxiety, which are intertwined with neurological well-being. It is also a leading cause of sleep apnea, a condition characterized by interrupted breathing during sleep. Sleep apnea can lead to fragmented sleep patterns and reduced oxygen supply to the brain. Over time, this may contribute to cognitive impairment. Understanding the intricate relationship between being overweight and neurological disorders is crucial to comprehensive health and well-being. By prioritizing weight management and adopting a balanced lifestyle, individuals can mitigate the risks associated with obesity and promote optimal brain function. As the saying goes, a healthy body leads to a healthy mind, and nurturing both aspects of our well-being is the key to a fulfilling life. Remember, small steps towards a healthier lifestyle can make a significant difference in the long run. Written by Caitlin Goodwin on Jan 21, 2021 Last reviewed and updated by Caitlin Goodwin on Oct 18, 2022 Caitlin Goodwin, DNP, RN, CNM, is a Board Certified Nurse-Midwife, Registered Nurse, and freelance writer. She has over twelve years of experience in nursing practice. Parkinson’s disease is a progressive nervous system disorder that affects movement. This neurodegenerative disorder affects cells in a specific area of the brain. According to the Centers for Disease Control and Prevention (CDC), the associated symptoms make Parkinson’s disease the 14th cause of death in the United States.
Parkinson’s disease causes stiffness or slowing of movement. It can start so gradually that it is often missed in the early stages. Empowering you and your family with information can help your family get an earlier diagnosis. This article will cover what to expect regarding Parkinson’s disease causes, symptoms, stages, diagnosis, and treatments. CausesThe cause of Parkinson’s Disease is mostly unknown. Those with Parkinson’s have low dopamine concentrations in their brain. However, some factors may increase the risk of Parkinson’s. Experts think that a combination of factors such as genetic mutations, lifestyle factors, and environmental effects cause the degenerative disorder. It is more likely to occur in men over the age of 60 years old. Chemicals like Trichloroethylene (TCEs) and Polychlorinated Biphenyls (PCBs) also increase the risk for Parkinson’s disease. SymptomsThe symptoms of Parkinson’s disease vary depending on how far the disease has progressed. Signs and symptoms are gradual and often start with a slight hand tremor. As the person with Parkinson’s advances along the spectrum, the signs and symptoms of the disorder worsen. Parkinson’s signs and symptoms include:
As the disease progresses, the following may occur as a result of the above symptoms:
Stages of Parkinson’s DiseaseThere are five stages of Parkinson’s disease.
DiagnosisDiagnosing Parkinson’s disease may be challenging as the symptoms are mild at first. There is no specific test that diagnoses the illness. A neurologist, a doctor specializing in nervous system conditions, will evaluate your case. If it is early in the process, a follow-up appointment may confirm worsening symptoms. The neurologist will ask questions like:
They will base their diagnosis on your medical history, signs, symptoms, and a neurological and physical exam. The neuro exam will cover mental status, balance, motor function, and a sensory exam. This will cover items like:
Your healthcare provider may order other tests, such as blood work or imaging like an MRI. However, instead of diagnosing Parkinson’s, these tests rule out other conditions that may be causing these symptoms. In rare cases, you may receive a dopamine transporter scan (DaTscan) to support the suspicion of Parkinson’s. Treatments There are many medical and surgical options for treatments for Parkinson’s, but no cure. Some medications will manage problems with walking, tremors, and movement by increasing dopamine. Dopamine cannot directly enter your brain. People with Parkinson’s disease have medication options:
Deep brain stimulation (DBS) is best for those with advanced Parkinson’s disease who have unstable responses to their drug regimen. However, it will not cure Parkinson’s nor stop it from advancing. Questions to Ask Healthcare Providers about Parkinson’s Disease Getting a diagnosis of Parkinson’s disease can seem overwhelming. For others, it may be helpful to finally understand the changes you’re experiencing. However, having a support network and working with your medical team is important. You should ask questions after the diagnosis, such as:
Bottom line While the cornerstone of Parkinson’s disease is worsening symptoms, there are ways to reduce them as the disease advances. The most crucial part of the treatment plan is a supportive network, coping tools, and safety measures. Coping tools include meditation, tai chi, yoga, or seeing a trusted therapist. If balance becomes a problem, it is crucial to prepare the bathroom with grab bars and remove rugs. An occupational therapist can help with other strategies to promote safety. Unfortunately, treatment cannot cure Parkinson’s disease, but you can manage the symptoms. Contact your healthcare provider or neurologist to start the conversation if you suspect that you or a loved one is symptomatic with Parkinson’s disease. If you have questions about performing CPR for those with dementia, Pacific ACLS provides courses and a guide to first aid for people with dementia to give you a more in-depth look. Works Cited
The attached PowerPoint is from Dr. Cokgor. She did a wonderful presentation on “Cryptogenic Stroke” last Wednesday. Cryptogenic Stroke definition is basically - An ischemic stroke occurring without being able to discover the cause/source. Crypto (hidden or secret) Genic (producing or forming) Meaning that what produced the stroke is unknown. Dr. Cokgor has several points that she wants to stress to us as nurses caring for the Cryptogenic Stroke Patient - Remember we do not know the cause for the stroke so……
View short videos regarding COVID-19 vimeo.com/showcase/6852479
|
|||||||||||||||||||||||||||||||||||||||||